Ever wondered what your bones are up to? Beyond simply holding you upright (a surprisingly challenging feat, if you think about it), your skeletal system is a complex, dynamic network, a silent symphony of calcium and collagen. But sometimes, this orchestra goes off-key, resulting in a range of conditions from the mildly inconvenient to the seriously debilitating. From the brittle fragility of osteoporosis to the creaky protests of osteoarthritis, we’ll explore the fascinating, and sometimes frankly bizarre, world of bone conditions and diseases.
Get ready to delve into the fascinating, sometimes alarming, and occasionally humorous reality of what goes on inside your bony framework.
This exploration will cover a variety of bone conditions, explaining their causes, symptoms, and treatments. We’ll journey through the intricacies of osteoporosis, the cartilage-crushing osteoarthritis, the genetic enigma of osteogenesis imperfecta, and the bone-remodeling rollercoaster of Paget’s disease. We’ll also tackle bone tumors, infections, fractures, and the often-overlooked duo of rickets and osteomalacia. Buckle up, it’s going to be a bumpy ride (pun intended!).
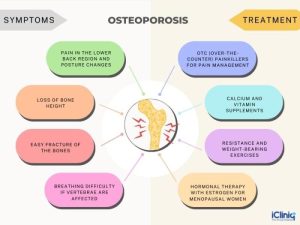
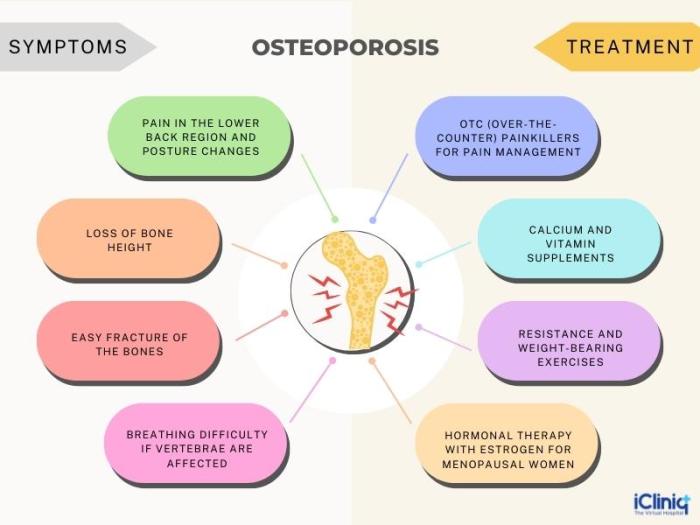
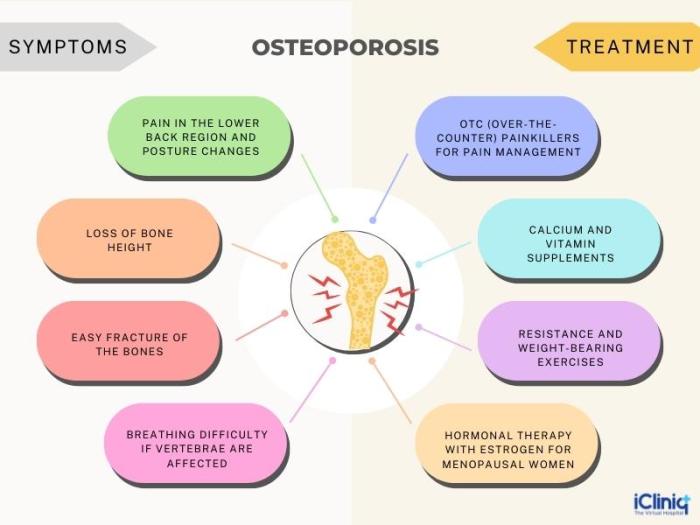
Osteoporosis
Osteoporosis, often dubbed the “silent thief of bones,” is a condition characterized by decreased bone mass and density, leading to increased bone fragility and a heightened risk of fractures. It’s a sneaky villain, often progressing without noticeable symptoms until a fracture occurs, which is why early detection and prevention are crucial. Think of your bones as a skyscraper – osteoporosis weakens the structural integrity, making it more vulnerable to collapse.
Osteoporosis Pathogenesis: A Bone-anza of Imbalance
Osteoporosis arises from an imbalance between bone resorption (the breakdown of bone tissue) and bone formation (the building of new bone). Normally, these processes are in a delicate equilibrium, constantly remodeling bone to maintain its strength and integrity. However, in osteoporosis, bone resorption significantly outpaces bone formation. This leads to a gradual loss of bone mass, making bones porous and susceptible to fractures.
Imagine a sculptor chipping away at a marble statue faster than they can add new marble – the statue becomes weaker and more fragile. Several factors contribute to this imbalance, including aging, hormonal changes (like menopause), genetics, and lifestyle choices.
Clinical Manifestations and Diagnostic Methods
Often, osteoporosis is asymptomatic in its early stages. The first sign is frequently a fracture, often occurring in the hip, spine, or wrist, even from a minor fall. Other potential, though less common, signs include back pain (due to vertebral compression fractures), loss of height, and stooped posture (kyphosis). Diagnosis typically involves a bone mineral density (BMD) test, often using dual-energy X-ray absorptiometry (DEXA).
This test measures the density of bone at specific sites (usually the hip and spine) and compares it to the bone density of a healthy young adult. A T-score (a standardized measure) helps classify the severity of osteoporosis. A T-score of -2.5 or lower indicates osteoporosis, while a T-score between -1.0 and -2.5 indicates osteopenia (low bone mass, a precursor to osteoporosis).
Blood tests may also be conducted to rule out other conditions and assess vitamin D levels, which play a vital role in bone health.
Treatment Plan for Osteoporosis: A Multi-pronged Approach
Managing osteoporosis requires a comprehensive approach that combines pharmacological and non-pharmacological interventions. The goal is to reduce fracture risk and improve bone health.
Pharmacological Interventions
Several medications are available to treat osteoporosis, each with its own mechanism of action and potential side effects. Choosing the right medication depends on various factors, including the patient’s age, overall health, and fracture risk.
| Medication Class | Medication Example | Mechanism of Action | Potential Side Effects |
|---|---|---|---|
| Bisphosphonates | Alendronate, Risedronate | Inhibit bone resorption | Esophageal irritation, jaw osteonecrosis (rare) |
| SERMs (Selective Estrogen Receptor Modulators) | Raloxifene | Mimic some effects of estrogen on bone | Hot flashes, blood clots (increased risk) |
| RANKL Inhibitors | Denosumab | Blocks bone resorption by inhibiting RANKL | Hypocalcemia, infections |
| Parathyroid Hormone Analogs | Teriparatide | Stimulates bone formation | Hypercalcemia, dizziness |
Non-Pharmacological Interventions
Lifestyle modifications play a crucial role in osteoporosis prevention and management. These include:* Regular Weight-Bearing Exercise: Activities like walking, jogging, dancing, and weight training help stimulate bone formation.
Adequate Calcium and Vitamin D Intake
These nutrients are essential for bone health. Dietary sources and supplements may be necessary.
Smoking Cessation
Smoking significantly increases the risk of osteoporosis.
Moderate Alcohol Consumption
Excessive alcohol intake can negatively impact bone health.
Fall Prevention Strategies
Home modifications and assistive devices can reduce the risk of falls and fractures.
Osteoarthritis
Osteoarthritis (OA), often called “wear and tear” arthritis, is a common joint disorder affecting millions worldwide. Unlike its more flamboyant cousin, rheumatoid arthritis, OA is a more subtle, insidious creep of joint degeneration, a slow dance of cartilage destruction that can leave you limping (metaphorically, hopefully!) years down the line. It’s a condition that affects the joints, primarily the weight-bearing ones like knees and hips, but can also target smaller joints in the hands and spine.Osteoarthritis Etiology and PathophysiologyOA’s underlying cause is a breakdown of the articular cartilage, the smooth, cushioning tissue that covers the ends of bones in a joint.
Imagine the cartilage as a perfectly smooth dance floor; in OA, that floor becomes cracked, pitted, and eventually worn away completely. This exposes the underlying bone, leading to pain, inflammation, and the formation of bone spurs (osteophytes). While aging is a major risk factor, the exact reasons for cartilage degradation remain somewhat mysterious. Genetic predisposition plays a role, as does joint injury (think that ill-fated soccer game from your youth).
Obesity also contributes significantly, as extra weight puts increased stress on the joints. Essentially, OA is a complex interplay of genetics, biomechanics, and aging, leading to a gradual deterioration of the joint’s protective cartilage.
Osteoarthritis Symptoms and Diagnostic Criteria
Common symptoms include joint pain, stiffness (especially after periods of inactivity), tenderness to the touch, limited range of motion, and the tell-tale crunching or grating sensation (crepitus) felt or heard when moving the affected joint. Diagnosis typically involves a physical examination, reviewing the patient’s medical history, and sometimes imaging tests like X-rays. X-rays can reveal characteristic features of OA, such as joint space narrowing (that worn-away dance floor!), osteophytes (those bony spurs), and subchondral sclerosis (hardening of the bone beneath the cartilage).
There’s no single blood test to definitively diagnose OA, unlike some other forms of arthritis. The diagnosis is largely based on clinical presentation and imaging findings.
Osteoarthritis Management Strategies
Managing OA focuses on pain relief, improving function, and slowing disease progression. There’s no cure, but many strategies can significantly improve quality of life.
Effective management strategies often involve a combination of approaches:
- Pain Management: This can include over-the-counter pain relievers like acetaminophen or ibuprofen, topical creams containing capsaicin, or stronger prescription medications such as opioids (used cautiously due to their potential for addiction) or NSAIDs (non-steroidal anti-inflammatory drugs) for more severe pain. In some cases, cortisone injections into the affected joint can provide temporary relief.
- Lifestyle Modifications: Weight loss is crucial for those who are overweight or obese, as reducing the load on the joints can significantly reduce pain and slow disease progression. Regular low-impact exercise, such as swimming, cycling, or walking, strengthens muscles supporting the joint and improves range of motion. Physical therapy can help improve joint mobility, flexibility, and strength. Assistive devices, such as canes or walkers, can also help reduce stress on affected joints.
- Surgical Interventions: For severe OA that doesn’t respond to conservative management, surgery may be an option. This can range from arthroscopy (a minimally invasive procedure to remove loose fragments of cartilage or bone) to joint replacement surgery (arthroplasty), where the damaged joint is replaced with a prosthetic. Joint replacement is a major surgery, but it can dramatically improve pain and function in severely affected joints.
For example, a patient with debilitating knee pain preventing them from walking comfortably might find a significant improvement in mobility after a knee replacement.
Osteogenesis Imperfecta

Osteogenesis imperfecta (OI), often called “brittle bone disease,” is a genetic disorder affecting collagen production, the crucial protein providing bones with their strength and flexibility. Imagine your bones as being made of slightly less sturdy LEGO bricks – prone to cracks and breaks under relatively minor stress. This isn’t just about clumsy tumbles; even everyday movements can cause fractures.
The severity of OI varies wildly, ranging from mild to severely debilitating.
Genetic Basis and Types of Osteogenesis Imperfecta
OI arises from genetic mutations affecting the genes responsible for type I collagen synthesis. These mutations can lead to a deficiency in collagen production, or the creation of faulty collagen molecules. This faulty construction results in weaker, more fragile bones. Different mutations lead to the various types of OI, categorized by their severity and associated features. The classification can be complex, but broadly, OI is classified into several types (I-VIII and beyond), primarily based on the severity of bone fragility, the presence of additional features like blue sclerae (the whites of the eyes appearing bluish), hearing loss, and the specific genetic mutation involved.
Type I, for instance, is a milder form, while Type II is the most severe, often leading to stillbirth or death in infancy.
Clinical Features and Diagnostic Approaches for Osteogenesis Imperfecta
The clinical presentation of OI is highly variable, depending on the type and severity. Common features include recurrent fractures, often occurring with minimal trauma. Many individuals with OI also experience short stature, skeletal deformities (such as bowed legs or arms), and a characteristically soft skull. The blue sclerae mentioned earlier are a striking feature in some types, caused by the thinness of the sclera allowing the underlying blood vessels to show through.
Hearing loss is another common complication, developing over time. Diagnosis typically involves a combination of clinical examination, genetic testing (to identify the specific gene mutation), and radiographic imaging (X-rays) to assess bone density and the presence of fractures. A detailed family history is also crucial, as OI often runs in families.
Management Strategies for Osteogenesis Imperfecta
Managing OI focuses on minimizing fractures, managing pain, and maximizing the individual’s quality of life. Supportive care includes physical therapy to improve strength and mobility, occupational therapy to adapt daily activities, and bracing to support weakened bones. Medications may be used to manage pain and reduce the risk of fractures. Bisphosphonates, for example, are frequently prescribed to increase bone density.
Surgical interventions may be necessary in some cases to correct severe deformities or stabilize fractures. These surgeries range from intramedullary rod placement (inserting rods into the long bones to provide support) to osteotomy (surgical cutting and reshaping of bone). Regular monitoring and a multidisciplinary approach involving orthopedists, geneticists, and other specialists are essential for effective management.
| Type | Bone Fragility | Other Features | Severity |
|---|---|---|---|
| Type I | Mild to moderate | Blue sclerae (often), hearing loss (later in life) | Mild |
| Type II | Severe | Severe bone fragility, often lethal in infancy | Severe |
| Type III | Severe | Progressive deformities, short stature, blue sclerae (often), hearing loss | Severe |
| Type IV | Moderate | Less severe than Type III, hearing loss (possible), blue sclerae (possible) | Moderate |
Paget’s Disease of Bone
Paget’s disease, also known as Paget’s disease of bone, is a chronic bone disorder where bone remodeling goes haywire – imagine a bone-renovating crew that’s both incredibly enthusiasticand* incredibly clumsy. Instead of building strong, sturdy bone, they create a chaotic mess of weak, misshapen bone. It’s not contagious (thank goodness!), and its cause remains a bit of a mystery, though genetics and viral infections are suspected players.
Paget’s Disease Pathophysiology
The core problem in Paget’s disease lies with the bone cells responsible for remodeling: osteoclasts (the demolition crew) and osteblasts (the construction crew). In Paget’s, the osteoclasts go into overdrive, resorbing bone tissue at an alarming rate. The osteoblasts, trying desperately to keep up, also work faster, but their efforts are disorganized and inefficient, resulting in the formation of weak, structurally unsound bone.
This leads to characteristic bone lesions that are enlarged, softened, and prone to fracture. Think of it like a poorly renovated house – the foundation is weak, the walls are uneven, and the whole thing is at risk of collapse. This chaotic cycle of excessive bone resorption and haphazard replacement contributes to the characteristic bone deformities seen in Paget’s disease.
Clinical Presentation and Diagnostic Methods
Paget’s disease often presents subtly, with symptoms sometimes absent altogether. When symptoms do appear, they vary widely depending on the location and severity of the bone lesions. Common symptoms include bone pain (often localized), bone deformity (leading to bowing of long bones or enlargement of the skull), and increased risk of fractures. In severe cases, neurological symptoms can occur due to bone compression on nerves.
Diagnosis typically involves imaging techniques like X-rays (showing characteristic lytic and sclerotic lesions), bone scans (detecting areas of increased bone turnover), and blood tests (revealing elevated levels of alkaline phosphatase, a marker of bone formation). A bone biopsy might be necessary in ambiguous cases to confirm the diagnosis.
Treatment Options for Paget’s Disease
The primary goals of treatment are to reduce bone pain, prevent fractures, and minimize complications. Bisphosphonates are the cornerstone of treatment. These drugs inhibit osteoclast activity, slowing down the excessive bone resorption. Calcitonin, another medication, can also help reduce bone turnover and alleviate pain. In some cases, surgery might be necessary to correct severe deformities or stabilize fractures.
The choice of treatment depends on the severity of the disease, the patient’s overall health, and the presence of complications.
Potential Complications of Paget’s Disease
The excessive bone turnover and structural weakening associated with Paget’s disease can lead to a number of serious complications.
- Fractures: The weakened bone structure is highly susceptible to fractures, even from minor trauma.
- Osteosarcoma: A rare but serious complication, Paget’s disease increases the risk of developing this type of bone cancer.
- Hearing loss: Involvement of the temporal bone can lead to conductive hearing loss.
- Cardiovascular complications: High output cardiac failure can occur due to increased blood flow through the affected bones.
- Neurological complications: Compression of nerves by enlarged bones can cause nerve pain, numbness, or weakness.
- Joint pain and arthritis: The bone deformities can lead to secondary osteoarthritis.
Bone Tumors
Bone tumors, those sneaky little (or sometimes not-so-little) residents of our skeletal system, can be a real bone of contention. They range from relatively harmless bumps in the road to aggressive invaders that demand immediate attention. Understanding the differences between benign and malignant tumors is crucial for effective treatment and, let’s face it, for keeping your bones happy.
Benign and Malignant Bone Tumors: A Tale of Two Tumors
Benign bone tumors are generally slow-growing and non-cancerous. They usually don’t spread to other parts of the body (metastasize), although they can sometimes cause problems due to their size or location. Think of them as the slightly annoying houseguest who overstays their welcome but ultimately isn’t destructive. Examples include osteochondromas (the most common type, often found in the long bones of the legs and arms, resembling a cauliflower-like growth), and giant cell tumors (usually found around the knee joint, and can be quite large).Malignant bone tumors, on the other hand, are cancerous and can spread to other parts of the body.
These are the unwelcome squatters who cause significant damage and require a full-scale eviction. They grow rapidly and can be very destructive to the bone. Examples include osteosarcoma (a highly aggressive cancer that often affects the long bones, particularly in adolescents and young adults), and Ewing sarcoma (a rare cancer that usually occurs in the bones of the arms, legs, or pelvis, often affecting children and young adults).
Diagnostic Methods for Bone Tumor Detection
Detecting bone tumors often involves a detective-like approach, utilizing various imaging techniques to get a clear picture of what’s going on inside those bones. X-rays provide a basic overview, revealing changes in bone density or structure. CT scans offer more detailed cross-sectional images, while MRI scans excel at visualizing soft tissues and bone marrow, providing a much clearer picture of the tumor’s extent.
Biopsies, involving the removal of a small tissue sample for microscopic examination, are essential for confirming the diagnosis and determining whether the tumor is benign or malignant.
Treatment Approaches for Bone Tumors
Treatment strategies for bone tumors depend heavily on several factors, including the type and location of the tumor, its size, and the patient’s overall health. Surgery is often the primary treatment for both benign and malignant bone tumors. This can range from simple removal of a benign tumor to more extensive procedures like limb salvage surgery (removing the tumor while preserving the limb) or amputation (in severe cases).
Chemotherapy, using powerful drugs to kill cancer cells, is a common treatment for malignant bone tumors, often used in conjunction with surgery or radiation therapy. Radiation therapy, using high-energy radiation to destroy cancer cells, can be used to shrink tumors before surgery or to kill any remaining cancer cells after surgery.
Comparison of Bone Tumor Types
| Tumor Type | Characteristics | Treatment | Prognosis |
|---|---|---|---|
| Osteochondroma | Benign, slow-growing, often asymptomatic | Observation, surgical removal if symptomatic | Excellent |
| Giant Cell Tumor | Benign, can be locally aggressive | Surgical removal, sometimes with adjuvant therapy | Generally good, but recurrence possible |
| Osteosarcoma | Malignant, highly aggressive, often metastasizes | Surgery, chemotherapy, radiation therapy | Variable, depends on stage and treatment response |
| Ewing Sarcoma | Malignant, can spread rapidly | Surgery, chemotherapy, radiation therapy | Variable, depends on stage and treatment response |
Bone Infections (Osteomyelitis)
Osteomyelitis: It sounds like a villain from a bone-themed superhero movie, doesn’t it? Unfortunately, it’s a very real and rather unpleasant bone infection. Let’s delve into the gritty details of this bone-gnawing foe.Osteomyelitis is a bone infection, usually caused by bacteria, that can lead to serious complications if left untreated. The bacteria reach the bone through the bloodstream (hematogenous spread), from a nearby infection (contiguous spread), or through direct introduction (e.g., during surgery).
Imagine a tiny Trojan horse of bacteria sneaking into the bone’s fortress, causing inflammation and damage. The body’s immune response tries to fight back, but sometimes the infection overwhelms it, leading to bone destruction and potential abscess formation. The mechanism involves the bacteria invading the bone marrow, disrupting blood supply, and causing inflammation and bone destruction. Different types of bacteria can cause osteomyelitis, with Staphylococcus aureus being a common culprit.
The severity depends on several factors, including the type of bacteria, the patient’s immune status, and the location of the infection.
Causes and Mechanisms of Osteomyelitis
The routes of infection are diverse and often depend on the individual’s circumstances. Hematogenous spread, where bacteria travel through the bloodstream, is common in children and individuals with underlying conditions like sickle cell anemia. This is because these conditions can compromise blood flow to the bone, making it more susceptible to infection. Contiguous spread, where the infection spreads from a nearby tissue, such as a wound or surgical site, is more frequent in adults.
Direct inoculation, such as from an open fracture or surgery, is another way bacteria can invade the bone. The body’s inflammatory response, while intended to fight off the infection, can ironically cause further damage by impairing blood flow to the affected area, leading to bone death (necrosis).
Clinical Presentation of Osteomyelitis
The symptoms of osteomyelitis can vary depending on the location and severity of the infection. Common symptoms include localized pain, swelling, redness, warmth, and tenderness at the affected site. Fever, chills, and fatigue are also common systemic symptoms. In children, osteomyelitis often presents with irritability, lethargy, and refusal to bear weight on the affected limb. Chronic osteomyelitis can lead to persistent pain, draining sinuses (holes in the skin), and bone deformities.
It’s important to note that the symptoms can be subtle, especially in individuals with weakened immune systems, making early diagnosis crucial.
Diagnostic Methods for Osteomyelitis
Diagnosing osteomyelitis requires a combination of clinical evaluation, imaging studies, and laboratory tests. Blood tests can reveal elevated white blood cell counts, indicating an infection. Imaging studies, such as X-rays, bone scans, MRI, and CT scans, are crucial for visualizing the extent of the infection. X-rays may not show changes in the early stages, but later stages will show bone destruction and bone loss.
Bone scans are highly sensitive to early infection. MRI provides detailed images of soft tissues and bone, while CT scans help to identify bone destruction and abscesses. In some cases, a bone biopsy might be necessary to identify the specific bacteria causing the infection and to determine the antibiotic sensitivity.
Treatment Strategies for Osteomyelitis
Treatment for osteomyelitis typically involves a combination of intravenous antibiotics and surgical debridement. Intravenous antibiotics are given for several weeks, sometimes months, to eradicate the infection. The choice of antibiotic depends on the type of bacteria identified. Surgical debridement involves removing infected bone and tissue to promote healing. In severe cases, surgical procedures may be needed to stabilize the bone, such as bone grafting or amputation.
For chronic osteomyelitis, long-term antibiotic therapy and repeated surgical debridement may be necessary. The overall goal of treatment is to eliminate the infection, preserve as much bone as possible, and restore function. Failure to adequately treat osteomyelitis can result in serious complications such as chronic pain, bone deformities, and even limb amputation.
Bone Fractures
Bone fractures, or broken bones, are a common injury, ranging from the mildly inconvenient to the seriously life-threatening. Think of your bones as incredibly strong yet surprisingly fragile structures – capable of supporting your weight but susceptible to damage from significant force. Understanding the different types of fractures and how they heal is key to effective treatment and recovery.
Types of Bone Fractures
Bone fractures are categorized in several ways, primarily based on the fracture’s appearance and the mechanism of injury. A simple fracture involves a break in the bone without damage to the surrounding skin, while a compound fracture (also known as an open fracture) pierces the skin, increasing the risk of infection. Further classification considers the fracture line’s configuration and location within the bone.
- Transverse Fractures: Imagine a clean break across the bone, like a perfectly straight line drawn across a ruler. These are often caused by direct force perpendicular to the bone.
- Oblique Fractures: These fractures run at an angle across the bone, like a diagonal slash. They usually result from a twisting or shearing force.
- Comminuted Fractures: Picture the bone shattering into multiple fragments. High-impact injuries are the usual culprits here, think car accidents or serious falls.
- Spiral Fractures: These fractures spiral around the bone, often seen in twisting injuries, such as a sports injury involving a sudden rotation of a limb.
- Greenstick Fractures: These fractures are incomplete breaks, most common in children whose bones are still relatively soft and pliable. Imagine bending a young, green twig – it cracks but doesn’t break completely.
- Avulsion Fractures: A piece of bone is pulled away from the main bone, usually by a strong muscle contraction. Think of a forceful tug on a tendon tearing a piece of bone away.
- Impacted Fractures: One end of the broken bone is driven into the other. This often occurs during falls, where the force of the impact compresses the bone.
Bone Fracture Healing
The healing process, a remarkable feat of biological engineering, involves several stages. Initially, a hematoma (blood clot) forms at the fracture site. This is followed by the formation of a callus, a soft tissue that bridges the gap between the broken bone ends. Over time, this callus gradually hardens and is eventually remodeled into new bone tissue, effectively knitting the fracture back together.
The entire process can take several weeks or even months, depending on the severity of the fracture and the individual’s health.
Treatment Approaches for Bone Fractures
Treatment options depend on the type and severity of the fracture, as well as the patient’s overall health.
- Casting: A cast, typically made of plaster or fiberglass, immobilizes the broken bone, allowing it to heal naturally. Imagine a sturdy protective shell encasing the injured limb.
- Splinting: A splint provides less rigid support than a cast and is often used for fractures that are not severely displaced or for initial stabilization before casting. Think of it as a more flexible, temporary support system.
- Surgery: Surgery may be necessary for complex fractures that require realignment (reduction) of the bone fragments or internal fixation (using plates, screws, or rods to hold the bones in place). This is particularly important for displaced fractures or those that are unlikely to heal properly without surgical intervention. For example, a comminuted fracture might necessitate surgery to stabilize the multiple bone fragments.
Rickets and Osteomalacia
Rickets and osteomalacia are both bone softening diseases, but they affect different age groups and manifest slightly differently. Think of them as mischievous siblings, both causing bone trouble, but with distinct personalities. Rickets affects growing children, while osteomalacia targets adults whose bones have already finished growing. Both, however, share a common thread: a deficiency in something crucial for strong bones.Rickets and osteomalacia share the common underlying cause of inadequate mineralization of the bone matrix.
This means the bones aren’t hardening properly, leading to softness and deformity. However, the age at which this occurs makes a significant difference in the clinical presentation. In rickets, the growing bones are affected, leading to characteristic deformities like bowed legs (genu varum), knock knees (genu valgum), and a widened wrist. Osteomalacia, on the other hand, typically presents with bone pain, muscle weakness, and increased risk of fractures in adults.
The bones themselves may not visibly deform as drastically as in rickets, but the increased fragility is a significant concern.
Vitamin D and Bone Health
Vitamin D plays a pivotal role in calcium absorption from the gut. Without sufficient vitamin D, the body struggles to absorb enough calcium, the essential building block for strong bones. This calcium deficiency is the primary reason why bones fail to mineralize correctly in rickets and osteomalacia. Other nutrients also contribute to bone health. Calcium itself is obviously critical, but phosphorus, magnesium, and vitamin K are also vital players in bone formation and maintenance.
A balanced diet rich in these nutrients is essential for preventing these conditions. Imagine your bones as a magnificent castle – vitamin D is the architect ensuring proper calcium absorption (the bricks), while other nutrients are the skilled craftsmen and laborers making sure everything is built correctly and strongly.
Treatment Strategies for Rickets and Osteomalacia
The cornerstone of treatment for both rickets and osteomalacia is vitamin D supplementation. The dose and duration of supplementation depend on the severity of the deficiency and the individual’s response to treatment. In severe cases, intravenous vitamin D may be necessary. Along with vitamin D, ensuring adequate calcium and phosphorus intake through diet or supplementation is crucial.
For children with rickets, addressing any underlying nutritional deficiencies and providing supportive care to correct bone deformities might also be needed. For adults with osteomalacia, pain management and strategies to reduce the risk of fractures are often part of the treatment plan. Regular monitoring of blood calcium and vitamin D levels is essential to ensure effective treatment and prevent recurrence.
Think of vitamin D supplementation as a magical potion that restores the bone’s ability to harden and become strong again.
Conditions and Diseases Affecting Bone Health (General Discussion)
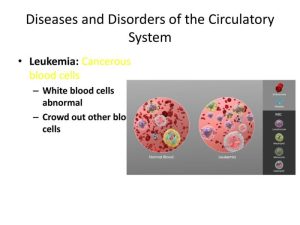
Our skeletal system, that magnificent internal scaffolding, isn’t just a collection of sturdy bones; it’s a dynamic, ever-changing organ system susceptible to a surprisingly wide array of conditions. While we’ve covered the big hitters like osteoporosis and osteoarthritis, the world of bone health is far from exhausted. Think of it like a bustling city – the main thoroughfares are well-known, but countless smaller streets and alleyways hold their own unique stories (and sometimes, their own unique bone-related dramas).Beyond the more common conditions, a fascinating menagerie of rarer bone diseases exists.
These can range from genetic disorders affecting bone formation to metabolic diseases that disrupt bone remodeling. Some, like fibrous dysplasia (where normal bone is replaced by fibrous tissue), might manifest as localized bone weakness, while others, like osteopetrosis (“stone bone”), lead to excessively dense and brittle bones. Understanding these rarer conditions is crucial for providing comprehensive care and highlighting the intricate complexity of bone health.
Rare Bone Diseases
Rare bone diseases often present unique challenges due to their low prevalence and varied clinical presentations. For example, enchondromatosis, a condition involving benign cartilage tumors within bones, can lead to bone deformities and fractures, requiring careful monitoring and tailored treatment plans. Similarly, osteochondroma, characterized by the growth of benign bone tumors near the ends of long bones, necessitates careful observation to detect any malignant transformation.
The clinical picture varies widely depending on the specific rare disease and its location and severity. Early diagnosis and appropriate management strategies are critical to minimize complications and improve patient outcomes.
Systemic Diseases and Bone Health
It’s a common misconception that bone health exists in a vacuum. In reality, our bones are deeply intertwined with the overall health of our bodies. Systemic diseases, those affecting the entire body, can significantly impact bone health. Diabetes, for example, is associated with increased risk of fractures due to impaired bone remodeling and reduced bone density. Similarly, chronic kidney disease can disrupt calcium and phosphate metabolism, leading to bone abnormalities like renal osteodystrophy.
These interactions highlight the importance of holistic healthcare approaches that consider the interconnectedness of different organ systems. Treating the underlying systemic disease is often crucial for improving bone health.
Preventative Measures for Bone Health
Maintaining strong, healthy bones throughout life is less about dodging landmines and more about building a solid foundation. Think of it as investing in a long-term project with incredibly high returns (a healthy, mobile you in your golden years!).A proactive approach to bone health should start early and continue throughout life. Here are some key lifestyle choices to strengthen your skeletal structure:
- Dietary Calcium and Vitamin D: These are the cornerstones of strong bones. Ensure adequate intake through diet or supplements.
- Weight-Bearing Exercise: Activities like walking, jogging, and weight training stimulate bone growth and increase density. Think of your bones as responding to stress like muscles.
- Healthy Lifestyle Choices: Maintaining a healthy weight, avoiding smoking, and limiting alcohol consumption all contribute to bone health. These choices are good for your whole body, including your bones.
- Regular Bone Density Checks: Especially important for those at higher risk, these tests can detect bone loss early, allowing for timely intervention.
Final Summary
So, there you have it – a whirlwind tour through the sometimes-fragile, sometimes-remarkably-resilient world of bones. While the prospect of bone diseases might initially seem daunting, understanding these conditions empowers us to take proactive steps towards maintaining skeletal health. Remember, your bones are your body’s silent workhorses, deserving of respect, care, and maybe the occasional calcium-rich treat. By understanding the intricacies of bone health, we can all strive to keep our skeletal systems in tip-top shape, ready to withstand the adventures life throws our way (even if those adventures involve the occasional tumble!).
Let’s raise a glass (of milk!) to healthy bones!
Question & Answer Hub
What’s the difference between a stress fracture and a regular fracture?
A stress fracture is a tiny crack in the bone, usually caused by repetitive stress, while a regular fracture is a complete break.
Can bone density be improved in adulthood?
Yes, through lifestyle changes like weight-bearing exercise, a balanced diet, and sufficient vitamin D and calcium intake.
Are all bone tumors cancerous?
No, many bone tumors are benign (non-cancerous). A biopsy is needed for definitive diagnosis.
How long does it typically take for a bone fracture to heal?
Healing time varies greatly depending on the type and location of the fracture, age, and overall health, but can range from weeks to months.
What are some early warning signs of osteoporosis?
Often, there are no early symptoms. Bone density scans are crucial for early detection.