Ever wondered what happens when your body’s amazing delivery service – the circulatory system – goes on strike? Picture this: tiny blood vessels, usually bustling with oxygen-rich red blood cells, suddenly turning into congested highways, causing a traffic jam of epic proportions. That’s the essence of circulatory system diseases – a captivating (and sometimes terrifying) tale of blockages, bursts, and general circulatory chaos.
This journey will explore the twists and turns of this vital system, from the sneaky villains like high blood pressure to the dramatic emergencies like strokes. Buckle up, it’s going to be a wild ride!
We’ll navigate the complexities of coronary artery disease (CAD), where plaque builds up like stubborn roadkill, clogging arteries and leading to chest pains and worse. We’ll witness the devastating impact of strokes, where blood flow to the brain is suddenly cut off, leaving behind a trail of neurological damage. We’ll also delve into the mysteries of heart failure, where the heart, our tireless pump, starts to falter.
This exploration will cover the various conditions, their causes, symptoms, treatments, and importantly, how to keep your circulatory system humming along like a well-oiled machine.
Introduction to Circulatory System Diseases
Your circulatory system – that amazing network of blood vessels and your tireless heart – is like a superhighway, constantly delivering vital supplies (oxygen, nutrients, the gossip from your liver) to every corner of your body and whisking away the waste products. Think of it as a 24/7, no-breaks delivery service, crucial for keeping you alive and kicking (or at least, not lying completely still).
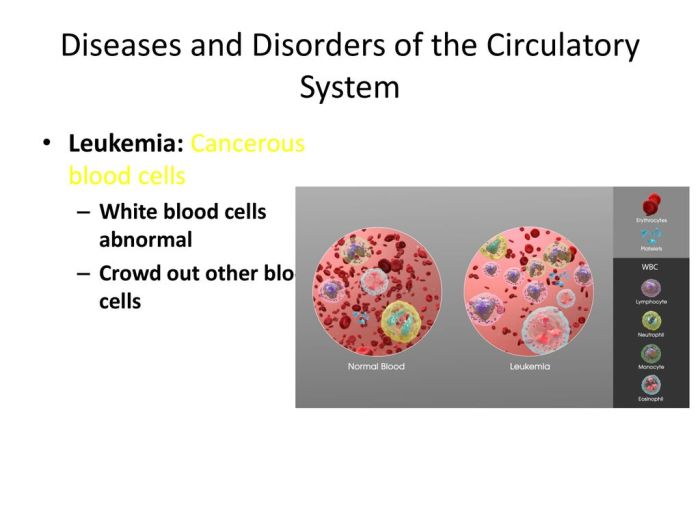
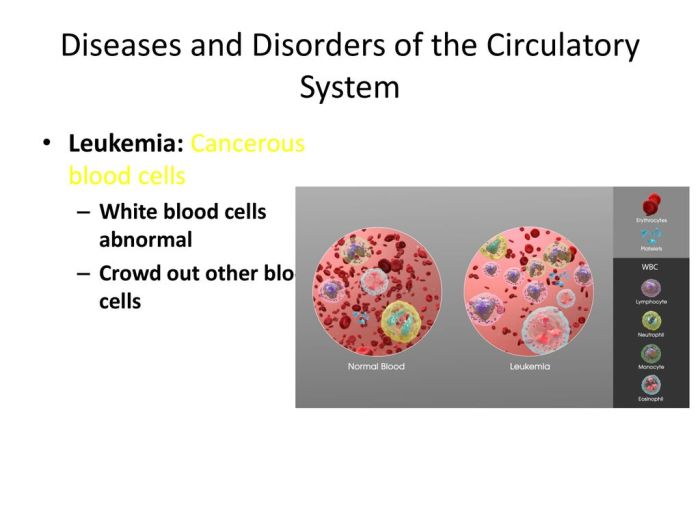
When this finely-tuned system falters, things get… messy.Circulatory system diseases encompass a wide range of conditions affecting the heart, blood vessels, and blood itself. These diseases, often interconnected and influenced by shared risk factors, can significantly impact quality of life and, in severe cases, lead to life-threatening complications. Understanding these diseases and their risk factors is crucial for prevention and early intervention.
Common Risk Factors for Circulatory System Diseases
Several factors significantly increase the risk of developing circulatory system diseases. These aren’t necessarily set in stone; many are modifiable through lifestyle changes. Ignoring these risks, however, is like playing Russian roulette with your heart (and not the fun kind).
- High Blood Pressure (Hypertension): The silent killer. High blood pressure puts extra strain on your blood vessels, increasing the risk of heart attack, stroke, and kidney failure. Imagine constantly inflating a balloon beyond its capacity – eventually, it’ll burst.
- High Cholesterol: Too much cholesterol, especially LDL (“bad” cholesterol), can clog your arteries, leading to atherosclerosis (hardening of the arteries). Think of it as slowly building up roadblocks on your circulatory superhighway, impeding traffic flow.
- Diabetes: High blood sugar damages blood vessels and nerves, increasing the risk of heart disease, stroke, and peripheral artery disease. It’s like adding sugar to your already overworked circulatory system – not a recipe for success.
- Smoking: Nicotine constricts blood vessels, raises blood pressure, and damages the lining of arteries. It’s a triple threat to your circulatory health, akin to intentionally throwing sand into the gears of your circulatory system.
- Obesity: Carrying extra weight puts a strain on the heart and increases the risk of developing other risk factors like high blood pressure and high cholesterol. It’s like overloading your delivery truck – eventually, it’ll struggle to make its rounds.
- Physical Inactivity: A sedentary lifestyle contributes to many of the risk factors mentioned above. Think of it as letting your circulatory system get rusty from lack of use.
- Family History: Genetics play a role. If your family has a history of heart disease, you’re at a higher risk. It’s like inheriting a slightly less reliable car model.
The Impact of Lifestyle Choices on Circulatory Health
Your lifestyle choices wield significant power over your circulatory health. Making positive changes can dramatically reduce your risk of developing circulatory system diseases. Think of it as a tune-up for your circulatory superhighway – regular maintenance prevents major breakdowns.Making healthy choices, like eating a balanced diet rich in fruits, vegetables, and whole grains; engaging in regular physical activity; maintaining a healthy weight; not smoking; and managing stress, is like performing regular maintenance on your circulatory system.
Conversely, neglecting these areas is akin to driving your car without oil changes or regular inspections. The result? A potential disaster waiting to happen. It’s an investment in your future, a chance to keep that circulatory superhighway running smoothly for years to come.
Coronary Artery Disease (CAD)
Coronary artery disease, or CAD, is essentially your heart’s plumbing system getting clogged. Think of it like a stubborn build-up of gunk in your pipes – only instead of dirty dishes, it’s cholesterol and other fatty deposits that narrow your coronary arteries, the vessels responsible for delivering life-giving oxygen to your heart muscle. This narrowing restricts blood flow, leading to a whole host of problems, from mild discomfort to major heart attacks.
It’s a leading cause of death worldwide, so understanding it is crucial.CAD develops gradually over time, often starting in childhood. The process, known as atherosclerosis, involves the formation of plaque within the artery walls. This plaque is a sticky mixture of cholesterol, fats, calcium, and other cellular debris. As the plaque builds up, it hardens and narrows the artery, reducing blood flow.
This process can be influenced by a variety of factors, including genetics, diet, smoking, high blood pressure, and diabetes – basically, many of the things your doctor nags you about. Sometimes, a plaque can rupture, triggering the formation of a blood clot that completely blocks the artery, leading to a heart attack. It’s a sneaky, silent thief that can creep up on you before you even realize it’s there.
Types of Angina
Angina is chest pain or discomfort caused by reduced blood flow to the heart muscle. It’s a common symptom of CAD, and its severity and characteristics can vary considerably depending on the extent of the blockage and other factors. Different types of angina are distinguished primarily by their onset, duration, and triggers.
Treatment Options for CAD
Treating CAD involves a multi-pronged approach, focusing on both lifestyle modifications and medical interventions. The goal is to improve blood flow to the heart, reduce symptoms, and prevent future cardiovascular events.
| Treatment Type | Description | Benefits | Risks |
|---|---|---|---|
| Lifestyle Modifications | Dietary changes (low fat, low cholesterol), regular exercise, smoking cessation, weight management, stress reduction techniques. | Improved overall health, reduced risk of disease progression, enhanced quality of life. | Requires commitment and adherence; may be challenging for some individuals. |
| Medications | Statins (to lower cholesterol), beta-blockers (to slow heart rate and lower blood pressure), nitrates (to dilate blood vessels), ACE inhibitors (to lower blood pressure), aspirin (to prevent blood clots). | Reduced risk of heart attack and stroke, improved blood flow, management of symptoms. | Side effects vary depending on medication; some medications may interact with other drugs. |
| Percutaneous Coronary Intervention (PCI) | A minimally invasive procedure where a balloon catheter is used to widen narrowed arteries; often combined with stent placement. | Immediate improvement in blood flow, reduced symptoms, lower risk of heart attack. | Bleeding, blood clots, allergic reactions to contrast dye, restenosis (renarrowing of the artery). |
| Coronary Artery Bypass Graft (CABG) | Open-heart surgery where a healthy blood vessel is grafted around a blocked coronary artery to restore blood flow. | Effective for severe CAD, improved long-term survival, relief from angina. | Higher risk of complications compared to PCI; longer recovery time; potential for surgical site infections. |
Stroke
Think of your brain as the CEO of your body – a vital organ orchestrating everything. A stroke is like a sudden, disastrous board meeting where the CEO gets unexpectedly incapacitated, leaving the entire operation in chaos. It’s a serious medical event that requires immediate attention.Stroke occurs when blood supply to part of the brain is interrupted or severely reduced, leading to brain cell damage.
This damage can result in a range of disabilities, depending on the area of the brain affected and the severity of the interruption. Time is of the essence in stroke treatment, as every minute counts in minimizing the damage.
Types of Stroke
Strokes are broadly categorized into two main types: ischemic and hemorrhagic. Ischemic strokes, the more common type, occur when a blood clot blocks blood flow to the brain. Imagine a clogged pipe preventing water from reaching its destination. Hemorrhagic strokes, on the other hand, happen when a blood vessel in the brain bursts, causing bleeding. Picture a pipe suddenly rupturing and flooding the surrounding area.
Both types lead to brain damage, but their causes and treatments differ significantly.
Signs and Symptoms of Stroke and the Importance of Timely Intervention
Recognizing the signs of a stroke is crucial for prompt treatment. The acronym FAST is a helpful mnemonic:
- Face drooping: Does one side of the face droop or feel numb?
- Arm weakness: Is there weakness or numbness in one arm?
- Speech difficulty: Is speech slurred or difficult to understand?
- Time to call 911: If you observe any of these signs, immediately call emergency services.
Other symptoms can include sudden severe headache, vision changes, dizziness, confusion, and loss of balance or coordination. The importance of timely intervention cannot be overstated. Rapid treatment, such as clot-busting drugs (for ischemic strokes), can significantly improve outcomes and reduce long-term disability. The window of opportunity for effective treatment is often narrow, emphasizing the critical need for immediate medical attention.
Stroke Prevention Strategies
Preventing a stroke involves adopting a healthy lifestyle. This includes managing risk factors such as high blood pressure, high cholesterol, diabetes, and atrial fibrillation (an irregular heartbeat). Regular exercise, a balanced diet low in saturated fat and sodium, and maintaining a healthy weight are essential. Quitting smoking is also crucial, as smoking significantly increases the risk of stroke.
Regular checkups with your doctor for monitoring blood pressure, cholesterol, and blood sugar are also highly recommended. Remember, prevention is always better than cure, especially when it comes to a condition as serious as a stroke.
Diagnostic Pathway for Stroke
A stroke diagnosis typically involves a rapid assessment by medical professionals, often beginning in the emergency room.
A flowchart illustrating the diagnostic pathway for stroke could be visualized as follows:
| Step | Action |
|---|---|
| 1 | Patient presents with suspected stroke symptoms (FAST signs). |
| 2 | Emergency medical services (EMS) are contacted; rapid transport to hospital. |
| 3 | Initial neurological examination to assess the severity of symptoms. |
| 4 | Non-contrast CT scan of the brain to differentiate between ischemic and hemorrhagic stroke. |
| 5 | If ischemic stroke is suspected, further imaging (e.g., CT perfusion, MRI) may be performed. |
| 6 | Blood tests to assess blood clotting factors and other relevant parameters. |
| 7 | Treatment initiated based on the type and severity of stroke. (e.g., thrombolytic therapy for ischemic stroke, surgical intervention for hemorrhagic stroke). |
| 8 | Ongoing monitoring and rehabilitation to manage complications and improve recovery. |
Heart Failure

Heart failure. Sounds dramatic, right? Like your heart’s throwing a pity party and refusing to work overtime. While it’s certainly a serious condition, understanding it can help demystify the process and, dare we say, make it a little less scary. Essentially, heart failure means your heart isn’t pumping blood as efficiently as it should, leading to a backup of blood and fluid in various parts of your body.
It’s not that your heart is failing completely – it’s more like it’s working overtime but not keeping up with the demands.Heart failure is broadly categorized into two main types: heart failure with reduced ejection fraction (HFrEF) and heart failure with preserved ejection fraction (HFpEF). Think of ejection fraction as the percentage of blood your heart pumps out with each beat.
In HFrEF, the heart muscle is weakened, resulting in a low ejection fraction (less than 40%), meaning it’s not pumping out enough blood. HFpEF, on the other hand, has a preserved or even normal ejection fraction, but the heart struggles to relax and fill properly, hindering its ability to pump blood effectively. Underlying causes are numerous and can include coronary artery disease, high blood pressure, heart valve problems, and even diabetes.
Essentially, anything that puts extra strain on your heart over time can contribute.
Types of Heart Failure and Their Underlying Causes
Heart failure isn’t a one-size-fits-all diagnosis. Different types arise from different underlying issues, impacting the heart’s ability to pump effectively. For example, damage from a heart attack can lead to HFrEF, while long-standing high blood pressure can contribute to HFpEF. Other causes include conditions affecting the heart valves, congenital heart defects, and diseases impacting the heart muscle itself.
The specific type and its severity depend on the underlying cause and the extent of damage to the heart.
Stages of Heart Failure Progression
Heart failure is often a progressive condition, meaning it can worsen over time. While the specific staging systems vary, they generally reflect the increasing severity of symptoms and the need for more aggressive treatment. Early stages might involve minimal symptoms, while later stages can be life-threatening, requiring intensive medical management. Think of it like a slow leak in a tire – you might not notice it at first, but eventually, it becomes a major problem.
Common Symptoms of Heart Failure
The symptoms of heart failure can vary depending on the severity and type. However, some common signs include:
- Shortness of breath, especially during exertion or when lying down (orthopnea).
- Persistent cough or wheezing.
- Fatigue and weakness.
- Swelling in the legs, ankles, and feet (edema).
- Rapid or irregular heartbeat (palpitations).
- Weight gain due to fluid retention.
- Reduced exercise tolerance.
Experiencing several of these symptoms warrants a visit to your doctor. Early diagnosis and treatment are crucial in managing heart failure and improving quality of life. Remember, heart failure is manageable, and with proper medical care, individuals can live fulfilling lives.
Peripheral Artery Disease (PAD)
Peripheral artery disease (PAD), also known as peripheral vascular disease, is like the circulatory system’s grumpy uncle who’s decided to clog up the plumbing in your legs and arms. It’s a condition where plaque buildup narrows your arteries, reducing blood flow to your extremities. Think of it as a traffic jam, but instead of cars, it’s your precious oxygen and nutrients struggling to get through.
This can lead to some serious discomfort, and if left unchecked, even more serious consequences.
PAD Pathophysiology
The root cause of PAD is atherosclerosis, the same villain responsible for many heart problems. This involves the gradual buildup of cholesterol, fatty substances, calcium, and other cellular debris within the artery walls, forming plaque. This plaque acts like a speed bump, significantly slowing down, or even completely blocking, blood flow. The reduced blood flow deprives tissues of oxygen and nutrients, leading to pain, cramping, and potentially tissue damage or even limb loss in severe cases.
Imagine your legs and arms complaining, “Hey! We’re not getting enough party favors (oxygen and nutrients)!”
Symptoms of PAD in Legs and Arms
PAD symptoms often vary depending on the location and severity of the blockage. In the legs, the most common complaint is intermittent claudication – a cramping pain in the legs and buttocks that occurs during exercise and is relieved by rest. It’s like your legs are saying, “Okay, I’m done with this marathon…for now!” This pain is usually felt in the calf muscles, but it can also occur in the thighs or buttocks.
In contrast, arm PAD symptoms are less common and may manifest as pain, numbness, or weakness in the arms or hands, particularly during exertion. Think of it as a less dramatic version of leg pain, but still a sign that something’s amiss. Severe PAD can lead to critical limb ischemia, characterized by severe pain, even at rest, skin ulcers, and gangrene – a truly unpleasant scenario.
Diagnostic Methods for PAD
Diagnosing PAD often begins with a thorough physical examination, including checking your pulse and listening to your arteries with a stethoscope. Doctors might also check your blood pressure in your arms and legs. Further investigations usually involve non-invasive tests like an ankle-brachial index (ABI) – a simple test comparing blood pressure in your ankles to your arms. A low ABI suggests PAD.
Doppler ultrasound imaging provides a visual representation of blood flow in your arteries, helping pinpoint the location and severity of blockages. Angiography, a more invasive procedure, involves injecting a dye into your arteries to visualize them through X-rays, providing a detailed map of your circulatory system.
Management Strategies for PAD
Managing PAD involves a multi-pronged approach, focusing on lifestyle modifications and medical interventions. Lifestyle changes are crucial and include regular exercise (especially walking!), quitting smoking (a major contributor to PAD), and adopting a healthy diet low in saturated fats and cholesterol. Imagine your arteries cheering you on as you make healthier choices! Medical therapies might involve medications to manage blood pressure, cholesterol, and blood clotting.
In more severe cases, procedures like angioplasty (balloon angioplasty to widen narrowed arteries) or bypass surgery (creating a detour around blocked arteries) may be necessary. These interventions help restore blood flow and alleviate symptoms. Think of it as a road crew clearing out that artery traffic jam.
Aneurysms
Imagine your blood vessels as a network of pipes carrying precious cargo – your blood. Sometimes, these pipes can weaken and bulge, forming a balloon-like swelling called an aneurysm. Think of it as a weak spot in the plumbing of your body, potentially leading to some serious plumbing issues. Aneurysms can occur in various parts of the circulatory system, each with its own set of quirks and complications.Aneurysms are essentially weakened areas in blood vessel walls that balloon outwards, increasing the risk of rupture.
The pressure of blood constantly pushing against this weakened area makes the aneurysm grow larger over time, and a larger aneurysm is more likely to rupture, which can be life-threatening. The location of the aneurysm determines the specific type and associated risks.
Types of Aneurysms
Several factors influence the development of aneurysms, including genetics, high blood pressure, smoking, and certain diseases like atherosclerosis. The most common types include aortic aneurysms (affecting the aorta, the body’s largest artery) and cerebral aneurysms (occurring in blood vessels in the brain). Other aneurysms can develop in other arteries throughout the body, though these are less common. The size and location of the aneurysm greatly impact its potential for rupture and the resulting complications.
Complications of Aneurysms
The most serious complication of an aneurysm is rupture. Imagine a balloon suddenly bursting – that’s what a ruptured aneurysm is like. A ruptured aortic aneurysm can lead to massive internal bleeding, often fatal. A ruptured cerebral aneurysm can cause a devastating stroke, leading to permanent brain damage or death. Even without rupture, aneurysms can cause pain, compression of surrounding tissues (leading to nerve damage or organ dysfunction), and the formation of blood clots.
The consequences of an aneurysm can be dire, highlighting the importance of early detection and treatment.
Diagnostic Procedures for Aneurysms
Detecting aneurysms often involves non-invasive imaging techniques. Ultrasound, a painless procedure using sound waves to create images of blood vessels, is frequently used for initial screening and monitoring. Computed tomography angiography (CTA) and magnetic resonance angiography (MRA) provide more detailed 3D images of blood vessels, allowing for precise assessment of aneurysm size and location. These advanced imaging techniques allow doctors to accurately visualize the aneurysm and plan the most appropriate treatment strategy.
Treatment Options for Aneurysms
Treatment options for aneurysms depend on several factors, including the aneurysm’s size, location, and growth rate. Small aneurysms that are not growing rapidly may be monitored closely with regular imaging. Larger aneurysms or those that are growing quickly often require intervention to prevent rupture. Surgical repair involves opening the chest or abdomen (in the case of aortic aneurysms) and replacing the weakened section of the artery with a graft.
Endovascular repair, a less invasive procedure, involves inserting a catheter through a blood vessel to place a stent-graft within the aneurysm, reinforcing the weakened area. The choice between surgical and endovascular repair depends on various factors, including the patient’s overall health and the specific characteristics of the aneurysm.
Hypertension (High Blood Pressure)
Hypertension, or high blood pressure, is a sneaky silent killer. It often shows no symptoms, meaning you could be unknowingly harboring this pressure cooker of a condition. Understanding its causes, consequences, and management is crucial for a healthy and long life, so let’s dive in!
Hypertension is essentially when the force of your blood against your artery walls is consistently too high. This puts extra strain on your heart and blood vessels, increasing your risk of serious health problems down the line. Think of it like constantly over-inflating a tire – eventually, it’s going to burst.
Causes and Consequences of Hypertension
The causes of hypertension are multifaceted and often involve a complex interplay of genetic predisposition and lifestyle factors. Some people are simply born with a higher risk due to family history, while others develop it due to unhealthy habits. These habits include things like a diet high in sodium (salt), lack of physical activity, obesity, excessive alcohol consumption, and chronic stress.
The consequences can be severe, ranging from stroke and heart attack to kidney failure and vision problems. Imagine your circulatory system as a complex network of pipes; high pressure damages those pipes over time, leading to all sorts of plumbing problems.
Primary and Secondary Hypertension
There are two main types of hypertension: primary (essential) and secondary. Primary hypertension accounts for the vast majority of cases and has no single identifiable cause. It’s the result of that complex interplay of factors mentioned earlier. Secondary hypertension, on the other hand, is caused by an underlying medical condition, such as kidney disease, sleep apnea, or certain medications.
Identifying the underlying cause is key to treating secondary hypertension effectively.
Monitoring and Managing Hypertension
Regular blood pressure monitoring is crucial for detecting and managing hypertension. This usually involves using a sphygmomanometer (that inflatable cuff and stethoscope combo). Doctors will typically use readings taken over several visits to establish a baseline. Management strategies involve lifestyle modifications (diet, exercise, stress reduction) and, often, medication. Think of it like fine-tuning a complex machine – a combination of adjustments is usually necessary to achieve optimal performance.
Blood Pressure Medications
Several classes of medications are used to treat hypertension, each working through different mechanisms. Choosing the right medication depends on individual factors and often involves a trial-and-error approach. It’s important to remember that side effects vary, and working closely with your doctor is essential.
| Medication Name | Class | Mechanism of Action | Side Effects |
|---|---|---|---|
| Lisinopril | ACE Inhibitor | Blocks the production of angiotensin II, a hormone that narrows blood vessels. | Dry cough, dizziness, fatigue |
| Hydrochlorothiazide | Thiazide Diuretic | Increases urine output, reducing blood volume. | Dehydration, electrolyte imbalance, dizziness |
| Amlodipine | Calcium Channel Blocker | Relaxes blood vessels, reducing blood pressure. | Headache, dizziness, swelling in ankles |
| Metoprolol | Beta-Blocker | Slows down heart rate and relaxes blood vessels. | Fatigue, dizziness, slow heart rate |
Conditions and Diseases Affecting Blood Vessels
Our circulatory system, that amazing highway of the body, relies on healthy blood vessels to keep things moving smoothly. But just like any highway system, things can go wrong. From tiny capillaries to major arteries and veins, blood vessels can be affected by a variety of conditions, leading to a range of symptoms and complications. Let’s explore some of these roadblocks in our body’s circulatory system.
These conditions often stem from inflammation, blockages, or weakening of the vessel walls. The underlying mechanisms can be complex, involving genetic predisposition, autoimmune responses, infections, and even lifestyle factors. Understanding these mechanisms is key to developing effective treatments and preventative measures.
Vasculitis
Vasculitis is an umbrella term for a group of diseases where the blood vessels become inflamed. Imagine your blood vessels as tiny, delicate pipes; in vasculitis, these pipes become irritated and swollen, restricting blood flow. This inflammation can affect vessels of various sizes, leading to different symptoms depending on the location and severity of the inflammation. Causes can range from infections to autoimmune disorders, where the body mistakenly attacks its own tissues.
Treatment often involves medications to suppress the immune system and manage inflammation, such as corticosteroids or immunosuppressants. In severe cases, surgery might be necessary to bypass blocked vessels.
Raynaud’s Phenomenon
Raynaud’s phenomenon is a condition where some blood vessels in the fingers and toes spasm, restricting blood flow. Think of it as a temporary, albeit sometimes painful, “traffic jam” in your extremities. This spasm causes the affected areas to turn white or blue, followed by a tingling or burning sensation as blood flow returns. While often triggered by cold temperatures or stress, the underlying cause can be idiopathic (meaning unknown) or secondary to other autoimmune diseases like lupus or rheumatoid arthritis.
Treatment focuses on managing triggers and improving circulation, including avoiding cold exposure, wearing warm clothing, and in some cases, medications to improve blood flow.
Atherosclerosis
While often discussed in the context of coronary artery disease, atherosclerosis is a broader condition affecting arteries throughout the body. It’s characterized by the buildup of plaque (cholesterol, fat, and other substances) within the artery walls. This plaque buildup narrows the arteries, reducing blood flow and increasing the risk of blood clots. Over time, this can lead to serious complications like heart attack, stroke, and peripheral artery disease.
Risk factors include high cholesterol, high blood pressure, smoking, diabetes, and family history. Treatment involves lifestyle modifications (diet, exercise, smoking cessation), medications to lower cholesterol and blood pressure, and in severe cases, procedures like angioplasty or bypass surgery to restore blood flow.
Congenital Heart Defects
Congenital heart defects (CHDs) are structural abnormalities of the heart present at birth. Think of them as little heart-shaped hiccups during fetal development – sometimes minor, sometimes requiring a bit more attention. These defects can range from relatively insignificant to life-threatening, depending on their severity and location. They’re surprisingly common, affecting approximately 1% of all newborns.Congenital heart defects encompass a wide array of issues affecting the heart’s structure.
These defects can involve the chambers (atria and ventricles), valves, great arteries (aorta and pulmonary artery), or the septa (walls) separating the heart’s different chambers.
Types of Congenital Heart Defects
Several examples illustrate the diversity of CHDs. Ventricular septal defects (VSDs) are holes in the wall separating the heart’s lower chambers (ventricles). Atrial septal defects (ASDs) are similar, but the hole is in the wall between the upper chambers (atria). Tetralogy of Fallot is a more complex defect involving four distinct abnormalities: a VSD, pulmonary stenosis (narrowing of the pulmonary artery), an overriding aorta (the aorta sits over both ventricles), and right ventricular hypertrophy (thickening of the right ventricle’s muscle).
Patent ductus arteriosus (PDA) is a condition where a blood vessel connecting the aorta and pulmonary artery during fetal development fails to close after birth. Transposition of the great arteries is a critical defect where the aorta and pulmonary artery are switched, leading to two separate circulatory systems.
Causes of Congenital Heart Defects
The exact cause of many CHDs remains unknown, but several factors are implicated. Genetic factors play a significant role; some CHDs are inherited, while others are caused by spontaneous gene mutations. Environmental factors during pregnancy, such as maternal infections (like rubella), exposure to certain medications, or uncontrolled diabetes, can also increase the risk. In some cases, a combination of genetic predisposition and environmental factors contributes to the development of a CHD.
For instance, a mother with a genetic predisposition to heart defects might have a higher risk of having a child with a CHD if she contracts rubella during pregnancy.
Consequences of Congenital Heart Defects
The consequences of CHDs vary widely depending on the specific defect and its severity. Minor defects may cause few symptoms, while major defects can lead to significant complications such as cyanosis (bluish discoloration of the skin due to low blood oxygen), heart failure, and developmental delays. Untreated CHDs can result in reduced oxygen levels in the blood, affecting various organs and systems.
In severe cases, untreated CHDs can be life-threatening. For example, untreated Tetralogy of Fallot can lead to “blue baby syndrome” due to severely low blood oxygen.
Diagnosis of Congenital Heart Defects
CHDs are often detected before birth through prenatal ultrasound scans. After birth, physical examination, electrocardiograms (ECGs – measuring the heart’s electrical activity), chest X-rays, and echocardiograms (ultrasound of the heart) are crucial diagnostic tools. Echocardiography provides detailed images of the heart’s structure and function, allowing doctors to pinpoint the exact location and nature of the defect. Cardiac catheterization, a more invasive procedure, may be necessary in some cases to further evaluate the defect and assess blood flow.
A fetal echocardiogram, performed during pregnancy, allows for early detection and planning for potential interventions after birth.
Treatment of Congenital Heart Defects
Treatment options range from watchful waiting for minor defects to complex surgical interventions for major ones. Medication may be used to manage symptoms and improve blood flow. Surgical repair is often necessary to correct structural abnormalities. In some cases, minimally invasive catheter-based procedures can be used to close small defects or widen narrowed arteries. The type of treatment will depend on the specific defect, its severity, and the patient’s overall health.
For example, a small VSD might close spontaneously, while a complex CHD like Tetralogy of Fallot would require surgical correction. Post-surgical care often involves medication to prevent complications and regular follow-up appointments to monitor the child’s progress.
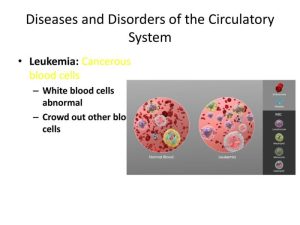
Infectious Diseases Affecting the Circulatory System
The circulatory system, that tireless postal service delivering oxygen and nutrients throughout your body, isn’t immune to unwanted visitors. Various infectious agents can wreak havoc on this vital network, leading to a range of potentially serious complications. Think of it as a microscopic invasion of the body’s express delivery system – a situation definitely not conducive to smooth operations!Infectious agents, ranging from bacteria to parasites, can access the circulatory system through various routes, leading to infections that can damage heart valves, blood vessels, and even the heart muscle itself.
These infections can range from relatively mild to life-threatening, depending on the infectious agent, the location of the infection, and the overall health of the individual. The body’s immune response, while usually effective, can sometimes be overwhelmed, leading to the need for aggressive medical intervention.
Bacterial Endocarditis
Bacterial endocarditis is a serious infection of the heart’s inner lining, usually affecting the heart valves. The culprits are typically bacteria, which can enter the bloodstream through various means, such as dental procedures, intravenous drug use, or infections elsewhere in the body. These bacteria then adhere to damaged areas of the heart valves, forming vegetations – essentially, bacterial colonies that can obstruct blood flow and potentially break off and travel to other parts of the body, causing emboli (blockages in blood vessels).
Symptoms can be subtle at first, mimicking other illnesses, but can progress to fever, fatigue, shortness of breath, and heart murmurs. Diagnosis involves blood cultures to identify the bacteria, echocardiography to visualize the heart valves and vegetations, and other imaging techniques. Treatment typically involves long courses of intravenous antibiotics, potentially requiring hospitalization. In severe cases, surgery may be necessary to repair or replace damaged valves.
Lyme Disease and the Circulatory System
Lyme disease, famously transmitted by the bite of infected blacklegged ticks, isn’t just a skin rash. The bacteriaBorrelia burgdorferi*, responsible for Lyme disease, can spread throughout the body, including the circulatory system. While the characteristic “bull’s-eye” rash is a common early symptom, later stages can involve inflammation of the heart muscle (myocarditis) and the membranes surrounding the heart (pericarditis), leading to irregular heartbeats, chest pain, and shortness of breath.
Lyme carditis, while relatively uncommon, can be serious and requires prompt treatment with antibiotics. Diagnosis involves a combination of blood tests, physical examination, and assessment of symptoms. Early diagnosis and treatment with antibiotics are crucial to prevent long-term complications. Delayed treatment can lead to chronic Lyme disease, with potential lasting effects on various organ systems.
Other Infectious Agents Affecting the Circulatory System
Several other infectious agents can affect the circulatory system, including fungi, viruses, and parasites. These infections can manifest in various ways, depending on the specific agent and the individual’s immune response. For instance, fungal infections can affect the heart valves, leading to conditions similar to bacterial endocarditis. Viral infections, such as those caused by certain viruses, can cause myocarditis, leading to inflammation and impaired heart function.
Parasitic infections are less common but can also involve the circulatory system, causing various complications. The diagnosis and treatment of these infections depend on the specific agent involved and may require specialized testing and therapies. Early detection and appropriate medical management are key to minimizing complications and improving outcomes.
Conclusive Thoughts
So, there you have it – a whirlwind tour of the circulatory system’s potential pitfalls. From the silent threat of hypertension to the dramatic flair of aneurysms, we’ve uncovered the fascinating (and sometimes frightening) world of circulatory diseases. Remember, knowledge is power, and understanding these conditions is the first step towards prevention and effective management. By making informed lifestyle choices and seeking timely medical attention, you can keep your heart and circulatory system happy, healthy, and ready for another adventure.
After all, a healthy circulatory system is the key to a vibrant life – think of it as the ultimate VIP pass to a long and fulfilling existence!
Answers to Common Questions
What’s the difference between a heart attack and a stroke?
A heart attack involves a blockage in the blood vessels supplying the heart muscle, while a stroke involves a blockage or rupture of blood vessels in the brain.
Can high blood pressure be cured?
While there’s no cure, hypertension can be effectively managed with lifestyle changes and medication, often keeping it under control for life.
Are all heart murmurs serious?
Not all heart murmurs indicate a serious problem. Some are innocent and harmless, while others can signal underlying heart conditions. A doctor’s evaluation is crucial.
How can I reduce my risk of developing circulatory diseases?
Maintain a healthy weight, exercise regularly, eat a balanced diet, don’t smoke, limit alcohol consumption, and manage stress effectively.