Ever wondered what goes on inside those amazing, air-conducting tubes called bronchi? They’re the unsung heroes of our breathing system, quietly doing their job until something goes wrong. Then, BAM! Coughing fits, wheezing, and a general feeling of “this air thing is not working as advertised.” This journey delves into the fascinating (and sometimes slightly terrifying) world of bronchial conditions, from the everyday sniffles to the more serious stuff.
Get ready for a whirlwind tour of coughs, wheezes, and all things bronchi!
We’ll explore the common culprits behind bronchial woes, from pesky infections to long-term conditions. We’ll unravel the mysteries of acute and chronic bronchitis, the curious case of bronchiectasis, and the surprisingly common (and sometimes misunderstood) bronchiolitis. Buckle up, because we’re about to explore the intricate network of tubes that keep us breathing—and what happens when things get a little… congested.
Introduction to Bronchial Conditions
Your lungs, those magnificent air-balloons keeping you alive, are a marvel of engineering. Air enters through your nose or mouth, travels down the windpipe (trachea), and then splits into two main branches – your bronchi, think of them as the main roads leading to your lungs’ many tiny air sacs (alveoli). These alveoli are where the magic happens: oxygen enters your bloodstream, and carbon dioxide exits.
The bronchi themselves are responsible for directing airflow, a job they perform with the help of tiny muscles and cilia (hair-like structures that sweep away mucus and debris). But, like any intricate system, things can go wrong.Bronchial diseases disrupt this carefully orchestrated air traffic control system, leading to a range of problems. These disruptions stem from various culprits, including infections (like the common cold or pneumonia, which can inflame the bronchi), irritants (such as cigarette smoke, air pollution, or allergens), and even genetic predispositions.
Some people are simply more susceptible to bronchial issues than others, due to factors beyond their control. Think of it as a traffic jam in your airways – sometimes it’s a minor fender bender, and other times it’s a major pile-up.
Severity and Symptoms of Bronchial Conditions
The severity of bronchial conditions varies wildly, ranging from mild annoyances to life-threatening emergencies. A simple cough might be the only symptom of a minor irritation, while a severe case of bronchitis could leave you gasping for air. Symptoms can include coughing (sometimes producing mucus), wheezing (a whistling sound during breathing), shortness of breath, chest tightness, and even fever.
The specific symptoms and their intensity depend on the underlying cause and the individual’s overall health. For instance, a person with asthma might experience wheezing and shortness of breath triggered by exposure to allergens, while someone with chronic bronchitis might experience a persistent cough with mucus production. The severity of symptoms can also fluctuate over time, even within the same individual.
A mild cold might trigger a temporary bout of coughing, while a flare-up of a chronic condition could lead to a more severe and prolonged episode.
Acute Bronchitis

Acute bronchitis: Think of it as your bronchi (the tubes leading to your lungs) throwing a hissy fit. It’s an inflammation of these airways, usually short-lived, and often leaves you feeling like you’ve wrestled a badger – and lost. It’s a common ailment, especially during cold and flu season, and while usually not serious, it can be incredibly uncomfortable.Acute bronchitis is primarily caused by viral infections, with the common cold virus being a frequent culprit.
However, bacterial infections can also be to blame, though less often. Irritants like cigarette smoke, air pollution, or even excessively dry air can also trigger an inflammatory response in the sensitive bronchial lining. Imagine your bronchi as delicate silk scarves – a harsh cough, irritating fumes, or a persistent viral attack can easily fray them.
Causes of Acute Bronchitis
Viral infections, such as the rhinovirus (responsible for many common colds), influenza viruses, and respiratory syncytial virus (RSV), are the most common causes. Bacterial infections, while less frequent, can also lead to acute bronchitis. Environmental irritants such as dust, fumes, and allergens can also trigger inflammation. Chronic exposure to irritants, like cigarette smoke, can significantly increase susceptibility.
Symptoms of Acute Bronchitis
The telltale signs of acute bronchitis often mimic a common cold, but with a focus on the chest. Expect a persistent cough, initially dry and later possibly producing mucus (phlegm) that can vary in color from clear to yellow or even green. This cough can be quite disruptive, keeping you awake at night and making even simple tasks challenging.
Other symptoms may include chest discomfort, shortness of breath (especially during exertion), and sometimes a low-grade fever. Fatigue is also common, leaving you feeling drained and generally unwell. Imagine trying to function while lugging around a heavy sack of potatoes – that’s the fatigue of acute bronchitis.
Treatment Approaches for Acute Bronchitis
Treatment for acute bronchitis focuses primarily on relieving symptoms and supporting the body’s natural healing process. Since it’s often viral, antibiotics are generally ineffective unless a bacterial infection is confirmed. Instead, rest is crucial – think of it as giving your body a chance to repair itself. Plenty of fluids help thin the mucus and ease coughing.
Over-the-counter medications like cough suppressants (for nighttime coughing) and expectorants (to help loosen mucus) can provide some relief. Humidifiers can add moisture to the air, soothing irritated airways. For severe cases or those with underlying health conditions, medical advice and potentially additional treatment may be necessary. A doctor might prescribe bronchodilators to help open the airways and make breathing easier.
Comparison with Other Respiratory Infections
Acute bronchitis shares some symptoms with other respiratory infections like pneumonia and the common cold. However, key differences exist. Unlike pneumonia, which involves inflammation of the lungs themselves, bronchitis primarily affects the bronchi. The common cold often presents with milder symptoms, primarily affecting the upper respiratory tract (nose and throat). While a cold might leave you with a sniffly nose and sore throat, bronchitis emphasizes the cough and chest discomfort.
Influenza (the flu) is another potential comparison. While both can cause coughing, the flu often includes more systemic symptoms such as high fever, body aches, and severe fatigue. Differentiating between these infections requires a medical assessment; self-diagnosis is not advisable.
Chronic Bronchitis
Chronic bronchitis: the long-term cough that just won’t quit. Imagine a persistent, nagging cough that sounds like a rusty swing set in a hurricane. That’s the essence of chronic bronchitis, a condition that makes breathing a daily battle. It’s not just a simple cold; it’s a chronic inflammatory disease that relentlessly attacks the airways, leading to significant long-term consequences.
Long-Term Effects on Lung Function
Chronic bronchitis relentlessly damages the lungs, leading to a cascade of problems. The airways become inflamed and narrowed, making it difficult to move air in and out. This persistent inflammation can lead to mucus buildup, further obstructing airflow and making breathing labored. Over time, the lung tissue itself can become damaged, reducing its ability to expand and contract efficiently.
This diminished lung function leads to shortness of breath, even during simple activities like walking up stairs. The constant struggle for air can also strain the heart, increasing the risk of heart failure. In severe cases, chronic bronchitis can lead to respiratory failure, requiring supplemental oxygen or even mechanical ventilation. Think of it as a marathon runner trying to finish the race with their lungs constantly filled with sand.
Risk Factors Associated with Chronic Bronchitis
Several factors significantly increase the risk of developing chronic bronchitis. Smoking is the biggest culprit, by far. The irritants in cigarette smoke directly inflame the airways and trigger chronic inflammation. Exposure to air pollution, whether from industrial emissions or vehicle exhaust, also plays a significant role. Genetic predisposition can make some individuals more susceptible to developing the condition.
A history of respiratory infections, particularly in childhood, can also increase the risk. Finally, working in environments with dust, fumes, or other respiratory irritants increases the likelihood of developing chronic bronchitis. These risk factors often work in tandem, creating a perfect storm for the disease.
Preventative Measures to Reduce Risk
While some risk factors, like genetics, are beyond our control, many others are modifiable. The single most effective preventative measure is quitting smoking. This action alone drastically reduces the risk of developing chronic bronchitis and other respiratory illnesses. Limiting exposure to air pollution is crucial; this can involve avoiding areas with high pollution levels, using air purifiers, and supporting policies that reduce emissions.
Practicing good respiratory hygiene, such as washing hands frequently and covering coughs and sneezes, can help prevent respiratory infections. Regular exercise strengthens the respiratory system and improves overall health. Finally, seeking medical attention for any persistent cough or respiratory symptoms is vital for early diagnosis and treatment.
Comparison of Acute and Chronic Bronchitis
| Symptom | Acute Bronchitis | Chronic Bronchitis |
|---|---|---|
| Cough | Usually productive (with mucus), often severe | Persistent, often productive, may be mild to severe |
| Chest Discomfort | May experience mild chest tightness or pain | May experience chest tightness, wheezing, and shortness of breath |
| Other Symptoms | Fever, fatigue, body aches, headache | Fatigue, shortness of breath, especially during exertion |
| Causes | Viral or bacterial infection | Smoking, air pollution, genetic predisposition, recurrent infections |
| Treatment | Rest, fluids, cough suppressants, bronchodilators (in some cases) | Smoking cessation, bronchodilators, inhaled corticosteroids, oxygen therapy (in severe cases) |
Bronchiectasis
Bronchiectasis: Think of your bronchi as a system of pipes carrying air to your lungs. In bronchiectasis, these pipes become permanently widened and damaged, a bit like old, leaky plumbing that’s seen better days. This leads to a chronic cough, often bringing up phlegm (mucus), and recurring respiratory infections. It’s not a pretty picture, but understanding it is the first step to managing it.
Pathological Changes in Bronchiectasis
The hallmark of bronchiectasis is irreversible dilation of the bronchi. Imagine the bronchial walls losing their elasticity and becoming weakened, leading to permanent enlargement and distortion. This damage often stems from recurrent infections that inflame and destroy the supporting tissues of the airways. The affected bronchi can become thick, inflamed, and filled with mucus, impairing airflow and creating a breeding ground for bacteria.
The resulting damage can lead to a variety of complications, including lung abscesses and bleeding. This isn’t just a little cough; it’s a structural alteration of the airways.
Diagnostic Methods for Bronchiectasis
Diagnosing bronchiectasis involves a detective-like approach. High-resolution computed tomography (HRCT) scans are the gold standard, providing detailed images of the airways to reveal their characteristic widening and changes. Chest X-rays can sometimes show abnormalities, but HRCT offers a much clearer picture. In addition, sputum cultures help identify the bacteria causing infections, guiding appropriate antibiotic treatment. Pulmonary function tests assess lung capacity and airflow, providing further insight into the extent of lung damage.
These tests, used in combination, paint a comprehensive picture of the disease’s severity and extent.
Management Strategies for Bronchiectasis
Managing bronchiectasis is a marathon, not a sprint, focusing on preventing and managing infections and improving lung function. Regular physiotherapy, including techniques like postural drainage and chest percussion, helps clear mucus from the airways. Antibiotics are crucial in combating bacterial infections, often prescribed prophylactically to prevent exacerbations. Bronchodilators can help relax the airways and improve breathing, while mucolytics thin the mucus, making it easier to cough up.
Lifestyle adjustments, such as quitting smoking and getting vaccinated against influenza and pneumonia, are essential in minimizing risk and improving overall health. These strategies aim to manage symptoms, prevent complications, and improve the patient’s quality of life.
Progression of Bronchiectasis: A Flowchart
Imagine a flowchart, starting with a recurring respiratory infection (like pneumonia or bronchitis). This initial infection can cause damage to the bronchial walls, initiating the process of bronchiectasis. Over time, this damage progresses, leading to the permanent widening of the bronchi. This persistent damage and the resulting airway obstruction create a vicious cycle: recurring infections become more frequent and severe, further damaging the bronchi.
Eventually, this can lead to various complications such as lung abscesses, hemoptysis (coughing up blood), respiratory failure, and even cor pulmonale (right-sided heart failure due to lung disease). This flowchart visually represents the chronic, progressive nature of the disease and the importance of early intervention.
Bronchiolitis
Bronchiolitis: It sounds like a villain from a cartoon, right? A tiny, mischievous gremlin wreaking havoc in your lungs? Well, while not quite a cartoon villain, bronchiolitis is a serious respiratory infection that primarily affects the smallest airways in your lungs – the bronchioles. Think of it as a miniature bronchitis, but with its own unique set of challenges.Bronchiolitis versus Bronchitis: A Tale of Two Infections.
Bronchitis inflames the larger airways (bronchi), while bronchiolitis targets the smaller ones (bronchioles). This seemingly small difference leads to significant variations in symptoms and severity. Bronchitis, while unpleasant, is often less severe, especially in healthy adults. Bronchiolitis, however, can be particularly dangerous for infants and young children, sometimes requiring hospitalization.
Populations Most Susceptible to Bronchiolitis
Bronchiolitis most commonly affects infants and young children, particularly those under six months old. Their smaller airways are more easily obstructed, and their immune systems are still developing, making them more vulnerable to severe infection. Premature babies and children with underlying heart or lung conditions are at even higher risk. Think of it like this: a tiny straw is much easier to clog than a large pipe.
Symptoms and Progression of Bronchiolitis
The symptoms of bronchiolitis usually begin subtly, often with a runny nose and mild cough. As the infection progresses, the cough worsens, becoming more frequent and often accompanied by wheezing. Babies might exhibit difficulty breathing, rapid breathing, and retractions (the skin pulling in around the ribs and collarbone during breathing). In severe cases, the child may appear lethargic, irritable, and have bluish discoloration of the skin (cyanosis) due to lack of oxygen.
The progression can be quite rapid, so it’s crucial to seek medical attention if you suspect your child has bronchiolitis. Imagine a slowly tightening knot in the airways, making each breath increasingly difficult.
Treatments for Bronchiolitis
The primary focus of bronchiolitis treatment is supportive care. There’s no magic cure, but several strategies help alleviate symptoms and prevent complications.
- Supportive Care: This involves ensuring adequate hydration, often through intravenous fluids if the child is unable to drink enough. Think of it as replenishing the body’s resources to fight the infection.
- Oxygen Therapy: Supplemental oxygen is provided to help maintain adequate oxygen levels in the blood, particularly in cases of severe respiratory distress. It’s like giving the lungs a little extra boost.
- Saline Nasal Aspirations: Clearing the nasal passages with saline solution can help improve breathing. It’s a simple yet effective way to clear the path for air.
- Medications: While antibiotics are generally ineffective against viral bronchiolitis, medications like bronchodilators may be used to help open the airways and reduce wheezing. These are not a cure but can help ease breathing difficulties.
- Monitoring: Close monitoring of the child’s respiratory rate, oxygen saturation, and overall condition is crucial to ensure timely intervention if needed. It’s like keeping a watchful eye on the situation.
Asthma and its Relation to Bronchial Health
Asthma, that mischievous little gremlin of the respiratory system, wreaks havoc primarily by targeting the bronchi. Think of your bronchi as the bustling highways of your lungs, carrying precious oxygen to and fro. In asthma, these highways become congested, inflamed, and prone to sudden, dramatic traffic jams. This leads to the characteristic wheezing, coughing, and shortness of breath that define an asthma attack.Asthma’s relationship with the bronchi is a close and often tempestuous one.
During an attack, the bronchial muscles tighten, constricting the airways. Simultaneously, the bronchial lining swells, further narrowing the passageways. This double whammy reduces airflow, making breathing feel like trying to suck air through a straw. Adding insult to injury, the airways become filled with extra mucus, further obstructing the flow of air. This is why understanding the bronchi’s role is crucial to managing asthma effectively.
Asthma Symptoms Compared to Other Bronchial Conditions
While asthma shares some symptoms with other bronchial conditions like bronchitis and bronchiectasis (cough, wheezing, shortness of breath), key differences exist. Bronchitis, for example, often features a more pronounced cough, frequently with mucus production, and may not necessarily involve the same degree of airway constriction as asthma. Bronchiectasis, a chronic condition, involves permanent widening and damage to the bronchi, resulting in persistent coughing and significant mucus production, unlike the episodic nature of many asthma attacks.
The hallmark of asthma is its reversible nature – with proper treatment, the airway constriction can be relieved, restoring relatively normal breathing. This reversibility is less pronounced or absent in chronic conditions like bronchiectasis.
Managing Asthma to Minimize Bronchial Inflammation
Effective asthma management focuses on minimizing bronchial inflammation and preventing attacks. This involves a multi-pronged approach. Firstly, identifying and avoiding triggers is crucial. Common triggers include allergens like pollen and dust mites, irritants like smoke and pollution, and even exercise or stress. Secondly, medication plays a pivotal role.
Inhalers, containing corticosteroids to reduce inflammation and bronchodilators to relax the airways, are cornerstones of asthma management. Regular use, even when symptom-free, helps prevent attacks. Finally, monitoring lung function through peak flow meters can provide valuable insights into the severity of the condition and the effectiveness of treatment. Regular check-ups with a pulmonologist are also essential to adjust treatment as needed and ensure the best possible bronchial health.
Tumors and Obstructions of the Bronchi

The bronchi, those vital airways branching off from the trachea, can unfortunately become the unfortunate victims of tumors and obstructions. These unwelcome guests can significantly disrupt the delicate balance of breathing, leading to a range of symptoms and complications. Let’s delve into the shadowy world of bronchial blockages and the bustling city of treatments designed to combat them.
Bronchial tumors, both benign and malignant, can significantly impact airflow and gas exchange. Benign tumors, while generally not cancerous, can still cause problems by physically blocking airways. Malignant tumors, or cancers, are far more serious, potentially metastasizing (spreading) to other parts of the body and disrupting lung function significantly. The location and size of the tumor heavily influence the severity of the resulting symptoms.
Obstructions aren’t limited to tumors; foreign bodies, inflammation, or even scar tissue can all contribute to airway blockage. The consequences are a reduction in oxygen intake and an increase in carbon dioxide retention, potentially leading to shortness of breath, coughing, wheezing, and even respiratory failure in severe cases.
Types of Bronchial Tumors
Bronchial tumors come in a variety of forms, each with its own set of characteristics and implications. The most common type is bronchogenic carcinoma, a lung cancer originating in the bronchial lining. These cancers are often categorized based on the type of cells involved (e.g., squamous cell carcinoma, adenocarcinoma, small cell carcinoma) and their stage (extent of spread).
Other, less common, tumors include benign lesions such as hamartomas (tumors composed of mature lung tissue) and carcinoids (neuroendocrine tumors). The characteristics of these tumors, such as their growth rate and invasiveness, dictate the treatment strategy.
Effects of Tumors and Obstructions on Airflow and Gas Exchange
The impact of bronchial tumors and obstructions on airflow and gas exchange is directly related to the location and severity of the blockage. A small tumor in a peripheral bronchus might cause minimal symptoms initially. However, a large tumor obstructing a major bronchus will drastically reduce airflow to a significant portion of the lung, leading to reduced oxygen uptake and impaired carbon dioxide removal.
This imbalance can lead to hypoxia (low blood oxygen levels) and hypercapnia (high blood carbon dioxide levels), causing symptoms like shortness of breath, cyanosis (bluish discoloration of the skin), and potentially respiratory failure. Other obstructions, like inhaled foreign bodies, can cause similar issues, depending on their size and location. A complete blockage can lead to collapse of the affected lung segment (atelectasis).
Treatment Options for Bronchial Tumors and Obstructions
Treatment for bronchial tumors and obstructions depends on several factors, including the type and size of the tumor or obstruction, the patient’s overall health, and the severity of symptoms. For benign tumors that are causing significant symptoms, surgical removal (bronchoscopic resection) may be an option. Malignant tumors, on the other hand, often require a more aggressive approach. Treatment options for lung cancer may include surgery (lobectomy, pneumonectomy), chemotherapy, radiation therapy, targeted therapy, and immunotherapy.
These treatments aim to shrink or eliminate the tumor and improve the patient’s quality of life. For obstructions caused by foreign bodies, bronchoscopy can be used to remove the obstruction. In cases of inflammation-induced obstruction, medications such as bronchodilators and corticosteroids can help alleviate symptoms and improve airflow. The choice of treatment is always individualized and tailored to the specific circumstances of each patient.
Infections Affecting the Bronchi
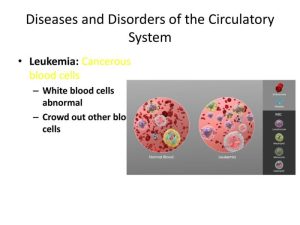
The bronchi, those crucial air-conducting tubes in our lungs, aren’t immune to the microscopic mayhem caused by infections. Just like a busy highway can get clogged with traffic, the bronchi can become congested with bacteria, viruses, and even fungi, leading to a range of unpleasant symptoms and potential complications. Let’s delve into the infectious villains that target these vital airways.
These infections trigger bronchial inflammation through various mechanisms. Bacteria, for instance, often release toxins that directly irritate the bronchial lining, causing swelling and increased mucus production. Viruses, on the other hand, can infect the bronchial cells themselves, leading to cell damage and inflammation. Fungal infections, though less common, can also cause significant bronchial inflammation through the release of inflammatory mediators and tissue invasion.
The body’s immune response, while intended to fight the infection, can also contribute to the overall inflammation.
Common Bacterial, Viral, and Fungal Infections
Bacterial infections are a frequent culprit in bronchial inflammation. Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis are common bacterial species implicated in acute bronchitis and other bronchial infections. Viral infections, particularly those caused by rhinoviruses, influenza viruses, and respiratory syncytial virus (RSV), are even more prevalent, often leading to milder infections but potentially paving the way for secondary bacterial infections.
Fungal infections of the bronchi are less common in healthy individuals but can occur in immunocompromised patients; Aspergillus species are among the fungi that can cause such infections.
Mechanisms of Bronchial Inflammation in Infections
The inflammatory response to bronchial infections is complex and involves multiple players. The invading pathogens trigger the release of inflammatory mediators such as cytokines and chemokines, which attract immune cells to the site of infection. These immune cells, including neutrophils and macrophages, attempt to eliminate the pathogens, but their activity can also contribute to the inflammation and tissue damage.
The increased mucus production, characteristic of many bronchial infections, further contributes to airway obstruction and the feeling of congestion. For example, in bacterial pneumonia, the inflammatory response can lead to fluid accumulation in the alveoli (the tiny air sacs in the lungs), causing significant respiratory distress. Similarly, viral bronchiolitis, particularly in infants, can lead to severe inflammation and airway obstruction due to the virus’s direct effect on the bronchioles.
Importance of Early Diagnosis and Treatment
Early diagnosis and treatment are paramount in preventing serious complications from bronchial infections. Prompt identification of the causative agent (bacterial, viral, or fungal) allows for targeted therapy, minimizing the duration and severity of the infection. Delaying treatment can lead to complications such as pneumonia, lung abscesses, and even respiratory failure, particularly in vulnerable populations such as the elderly, young children, and individuals with underlying lung conditions.
For instance, untreated bacterial bronchitis can progress to pneumonia, requiring hospitalization and potentially more aggressive treatment with intravenous antibiotics. Early intervention with appropriate antibiotics or antiviral medications, along with supportive care, can significantly improve outcomes and prevent these serious complications.
CONDITIONS AND DISEASES: A Broader Perspective
Our journey through the bronchial tree has been, shall we say,thorough*. We’ve tackled the individual villains – bronchitis, bronchiectasis, and the surprisingly mischievous bronchiolitis – but now it’s time to zoom out and appreciate the grand, sprawling landscape of respiratory conditions. Think of it as going from meticulously examining a single leaf to appreciating the majesty of the entire forest.
This section will explore the wider world of respiratory diseases, highlighting their commonalities, differences, and the often-overlooked role of our environment.The respiratory system, that amazing air-processing plant inside us, is constantly battling a barrage of threats. These threats range from microscopic invaders like viruses and bacteria to larger irritants such as pollutants and allergens. Understanding how these different threats manifest themselves is key to understanding the diverse spectrum of respiratory illnesses.
We can broadly categorize these illnesses based on whether they’re primarily obstructive (blocking airflow), restrictive (limiting lung expansion), or a combination of both.
Obstructive Lung Diseases
Obstructive lung diseases, as the name suggests, make it difficult to exhale fully. Think of it like trying to squeeze toothpaste out of a tube that’s almost completely clogged. Asthma, chronic bronchitis, and emphysema are prime examples. These conditions often involve inflammation and narrowing of the airways, hindering the smooth flow of air. The underlying causes vary; asthma is often triggered by allergies or irritants, while chronic bronchitis is frequently linked to long-term exposure to irritants like cigarette smoke.
Emphysema, on the other hand, involves the breakdown of the tiny air sacs in the lungs, making exhalation even more challenging.
Restrictive Lung Diseases
In restrictive lung diseases, the lungs’ ability to fully expand is compromised. Imagine trying to inflate a balloon that’s been tightly wrapped in cling film. Conditions like pulmonary fibrosis (scarring of lung tissue), sarcoidosis (formation of inflammatory granulomas), and some forms of neuromuscular diseases fall under this category. These conditions can significantly reduce lung capacity, leading to shortness of breath and reduced oxygen intake.
The causes are diverse, ranging from genetic factors and autoimmune responses to exposure to certain environmental toxins like asbestos.
Environmental Factors and Respiratory Health
The air we breathe is not always our friend. Air pollution, a cocktail of noxious gases and particulate matter, is a significant contributor to various respiratory problems. Exposure to pollutants can trigger inflammation, exacerbate existing conditions like asthma, and even contribute to the development of chronic lung diseases. This isn’t just a problem in industrial areas; even seemingly clean air can contain pollutants from vehicle emissions, wildfires, and other sources.
Furthermore, allergens such as pollen, pet dander, and dust mites can trigger allergic reactions leading to asthma attacks, rhinitis, and other respiratory symptoms. Occupational hazards, such as exposure to asbestos or silica dust, can lead to serious and potentially fatal lung diseases. Consider the case of asbestos miners in the past, many of whom developed asbestosis, a severe and debilitating lung disease, highlighting the significant impact of environmental factors.
Similarly, the rise in respiratory illnesses in urban areas compared to rural areas directly reflects the increased exposure to pollutants in densely populated areas.
Final Summary
So, there you have it – a whistlestop tour of the bronchial world! From the everyday sniffles of acute bronchitis to the more serious challenges of bronchiectasis, understanding our bronchi is key to maintaining good respiratory health. Remember, prevention is always better than cure, so look after those airways – they’re doing a lot of heavy lifting for you every single day.
And if something feels amiss? Don’t hesitate to consult a medical professional – they’re the real experts in navigating this sometimes tricky terrain.
Popular Questions
What’s the difference between a cough from bronchitis and a cough from something else?
A bronchitis cough is often persistent and can produce mucus. Other coughs might be dry, short-lived, or associated with other symptoms like fever or a runny nose. Only a doctor can definitively diagnose the cause.
Can bronchitis be prevented?
While you can’t completely prevent bronchitis, practicing good hygiene (handwashing!), avoiding exposure to irritants (like smoke), and getting enough rest can significantly reduce your risk.
Are all bronchial conditions serious?
No, many bronchial conditions are relatively mild and easily treated. However, some, like bronchiectasis, can be chronic and require ongoing management. Early diagnosis is crucial.
How is bronchiectasis diagnosed?
Diagnosis often involves a combination of chest X-rays, CT scans, and tests to analyze sputum (mucus coughed up from the lungs).